Individuals who identify as transgender and non-binary may no longer use their birth or legal name but rather choose a new name that aligns with their identity. When they ask that you use their new name instead, calling them by their old name is referred to as deadnaming and can be a stressful and traumatic experience for the individual and is even considered an act of verbal violence.
In the healthcare setting, however, you may encounter situations where a patient has communicated a chosen name but has not legally changed it, so the deadname is reflected in their medical record. In those instances, completing the patient identification (ID) by confirming their name with their medical record/patient ID band may result in inadvertent deadnaming.
Policies and Procedures to Prevent Deadnaming
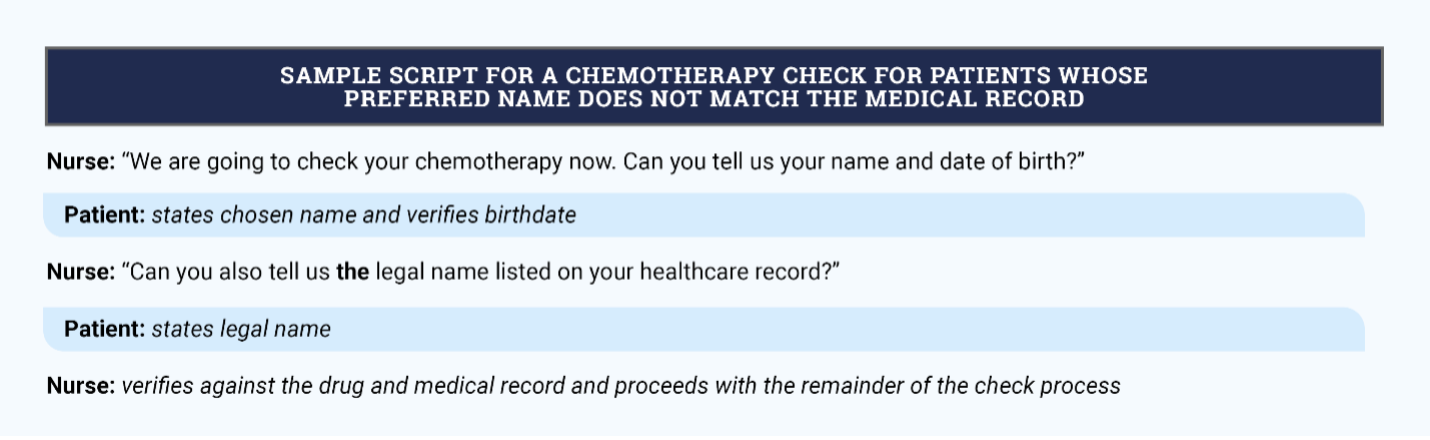
Healthcare facilities must provide guidance for completing safety checks such as patient ID and chemotherapy/biotherapy checks for patients whose preferred name is not the same as the name on their medical record. Policies and procedures should guide healthcare workers to:
- Educate patients on your desire to respect their wishes and keep them safe while they are in your care.
- Ask patients to state their chosen name and the legal name on the record so that it can be verified against the orders. Using the verbiage “the” legal name, not “your” legal name, separates the name from the individual.
- Reinforce that you recognize that the name on the medical record is not their name, but it is a part of the safety check process at this time.
- Work with your leadership and technology services to explore opportunities to capture the patient’s preferred name in the medical record.
See the sidebar for an example of a script for a chemotherapy check.
If you accidentally deadname someone during care delivery, follow the three A’s for resolution:
- Acknowledge your mistake.
- Apologize to the individual, even if time has passed. Don’t make an excuse or dismiss it.
- Actively work toward not repeating the event.
Have you experienced a cultural clinical practice encounter or situation that would be helpful for other oncology nurses to understand? Email us about it at pubONSVoice@ons.org for consideration for a future article.
Acknowledgement: We thank ONS member Beau Amaya, MSN, RN, OCN®, Safe Zone trainer, for contributing to the development of this article.






