Communication Models Help Nurses Confidently Address Sexual Concerns in Patients With Cancer
Sexual dysfunction is one of the most common side effects of cancer treatment, yet oncology professionals often under address patients’ sexuality and sexual dysfunction concerns (https://doi.org/10.1200/EDBK_100032). Providers cite lack of time, training, and resources (https://ascopost.com/issues/june-25-2021/addressing-sexuality-challenges-throughout-the-cancer-care-continuum/) as barriers to initiating important discussions about sexual side effects, and studies show that patients’ age and prognosis (https://doi.org/10.1007/s13187-019-01559-6) are additional hindering factors.
Sexual side effects may not be a concern or recognized early in the treatment course (https://doi.org/10.1200/EDBK_100032), but when they surface during survivorship (https://doi.org/10.1200/EDBK_100032), patients may confide in oncology nurses (https://ascopost.com/issues/june-25-2021/addressing-sexuality-challenges-throughout-the-cancer-care-continuum/) and social workers to address their most intimate matters. Educational training programs and reliable resources can empower oncology nurses to confidently address patients’ and their partners’ sexual concerns.
Resources for Addressing Sexuality and Intimacy Issues
Outcomes from sexual health education workshops have shown that nurses’ confidence levels increase significantly when they gain knowledge and awareness of sexual health resources, with one educational intervention showing sustained effects at six months. The use it or lose it and practice makes perfect adages apply to increasing confidence levels over time (https://doi.org/10.4324/9781315648682-4) when initiating conversations about sexuality and intimacy in oncology care.
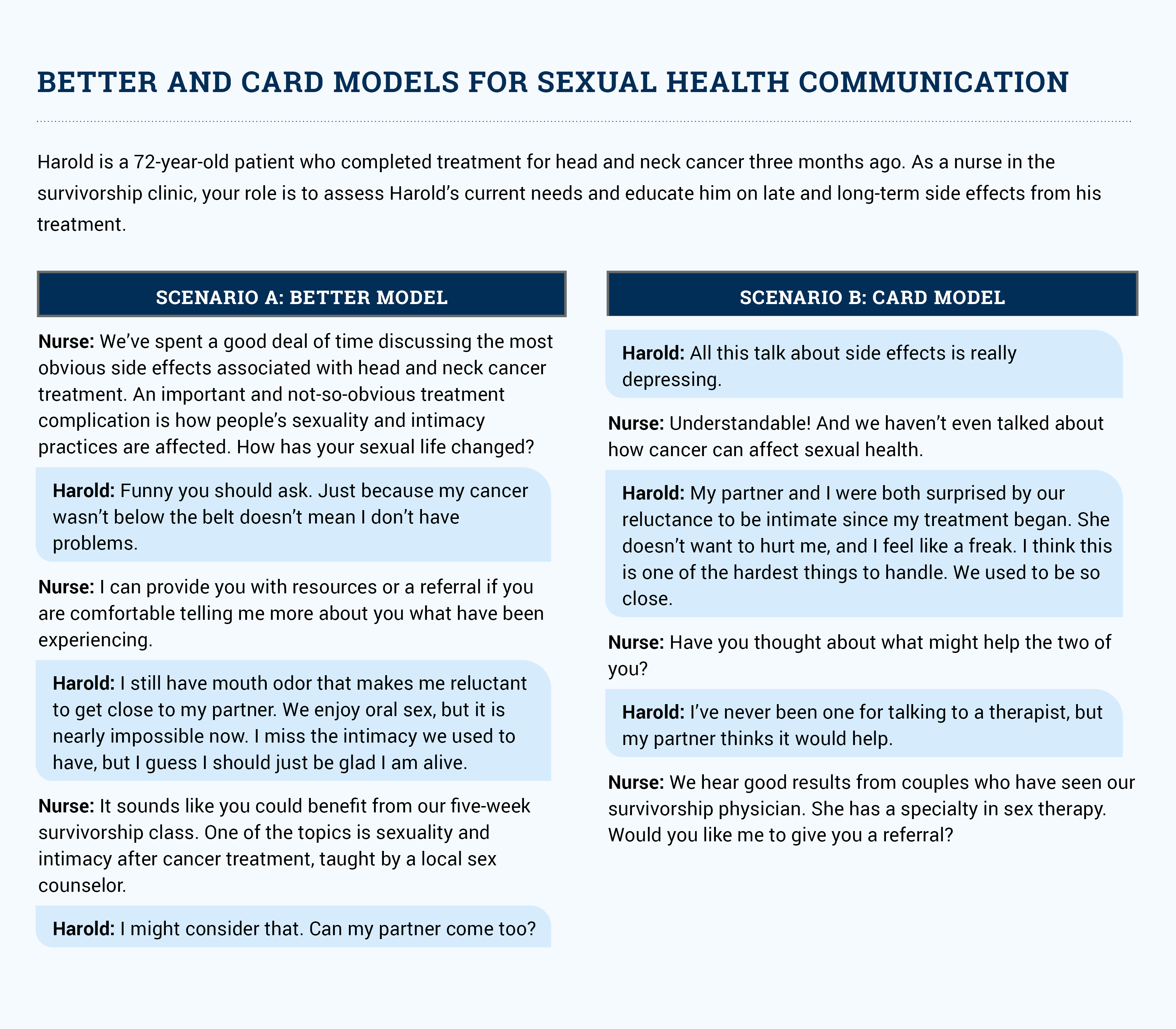
Several models, including BETTER, CARD, and PLISSIT (https://www.researchgate.net/publication/338518344_Application_of_the_Extended-PLISSIT_Model_to_Improve_Sexual_Health_in_the_Adolescent_Population_A_Theory_Analysis), can help nurses facilitate sexual health communication. The BETTER model (https://doi.org/10.1188/04.CJON.84-86) has six steps:
- Bring it up
- Extinguish embarrassment by normalizing the topic
- Tell the listeners that resources will be provided
- Respect the time a person is willing to spend
- Educate
- Record (document) the interaction
The CARD model (https://doi.org/10.4324/9781315648682-4)’s four steps are similar:
- Explain that cancer can affect sexual health
- Ask if they have any questions about sexual health
- Provide resources and referrals
- Document
The scenarios in the sidebar show you how to use the BETTER and CARD models in your patient interactions.