Quality cancer care requires safety, efficacy, timeliness, and a patient-centered approach coordained by an interprofessional team with the integration of evidence-based practices to continuously improve care. Holistic, culturally sensitive, quality cancer care [also] requires equitable access to healthcare professionals via telehealth or in-person visits across specialties with an understanding of how cancer and cancer treatments affect wellness.
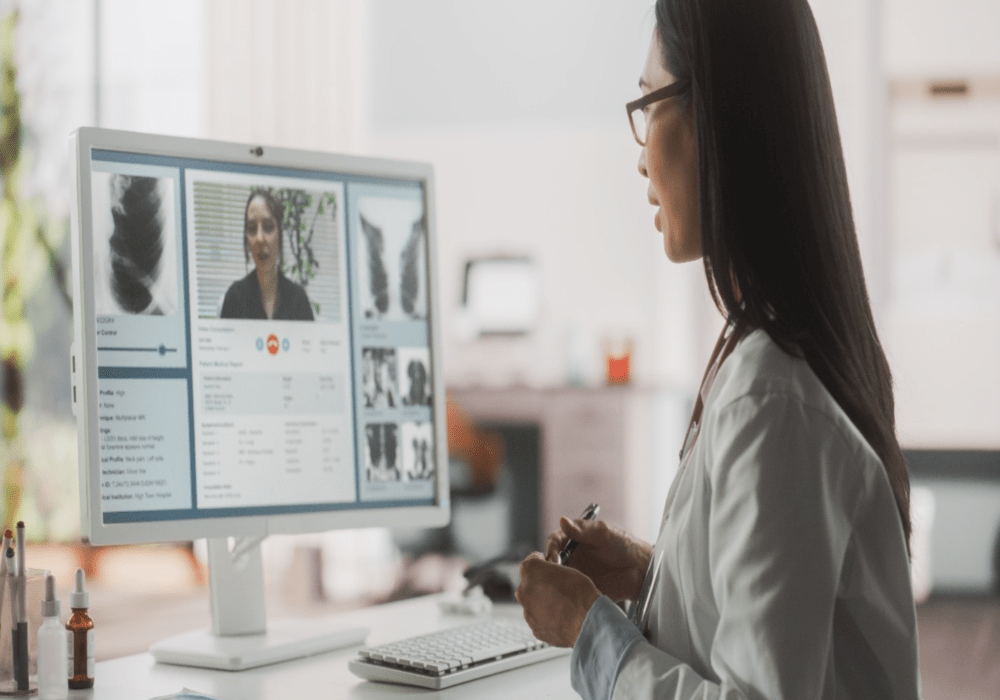
Telehealth, telemedicine, and virtual health have come a long way from the days of telephone triage. No longer just a voice on the other end of the line, today’s technologies connect patients and providers face to face, regardless of location. With an eye toward patient-centered care, the advantages of a virtual environment include shorter appointment wait times, less risk for immunocompromised patients, and coordinated care with caregivers and family members.
Telehealth Diminishes Digital Divides
Driving innovation and best practices, the American Nurses Association outlined 13 key nursing tenets in its Core Principles on Connected Health. Grounded in the Nurses Code of Ethics, several principles support ONS’s stance in its Access to Quality Cancer Care position statement:
- The use of connected health technologies does not alter the standards of professional practice when delivering health care, conducting research, or providing education.
- Healthcare services delivered via connected health technologies should prioritize improving access to quality health care that is guided by best available evidence, accepted clinical standards, and best practices.
- To inform connected health and ensure the best outcomes, it is essential that the assessment, evaluation, and study of all aspects of connected health are ongoing and systematic.
The underlying message from both organizations is that telehealth and other connected health services enable nurses to provide safe, effective, efficient, and evidence-based patient-centered care and symptom management education.
Legislative Leadership Brings Telehealth to the Masses
Like so much in the healthcare system, telehealth’s further expansion revolves around money. Can a provider bill for a virtual consult? How do we bill with multiple accounting and privacy systems that do not communicate? Should a virtual conversation incur the same rate as an in-person office visit?
Seizing on public interest, legislators around the country are introducing bipartisan bills with telehealth components. In 2023 alone, the 118th Congress has considered:
- H.R. 3432, the Telemental Healthcare Access Act of 2023, which ensures coverage of mental and behavioral health services delivered through telehealth
- H.R. 1843, the Telehealth Expansion Act of 2023, which permanently extends the exemption for telehealth services from certain high-deductible health plan rules
- S. 729, the Audio-Only Telehealth for Emergencies Act, which waivers certain telehealth requirements to permit reimbursement for audio-only telehealth services under the Medicare program during emergency declarations
- H.R. 3440, the Protecting Rural Telehealth Access Act, which protects access to telehealth services under the Medicare program
- S. 2016, which amends title XVIII of the Social Security Act to expand access to telehealth services
“Telehealth has proven its worth and effectiveness in increasing access to care for millions of Americans living in rural communities. Congress should build on that success to ensure these vulnerable populations can continue to access innovative and lower-cost care. The Telehealth Expansion Act of 2023 will allow millions of Americans to continue accessing telehealth before meeting their deductible—an important step in keeping common sense health care tools in place for those who need them,” U.S. Representative Jason Smith (R-MO), chair of the House Committee on Ways and Means, said.
Agencies and Acts Support Patients and Providers
The Health Resources and Services Administration (HRSA) agency touts tangible telehealth tickers. With a mission to “improve quality health care through integrated telehealth services,” its Office for the Advancement of Telehealth has more than 5 million users of telehealth.HHS.gov and more than 6,000 telehealth technical assistance requests in its resource centers, all of which reaches more than 22,000 patients in its network.
Today’s legislative and regulatory agenda also focuses on helping employers provide benefits for their healthcare workers. In June 2023, the U.S. House Committee on Education and the Workforce passed H.R. 824, the Telehealth Benefit Expansion for Workers Act of 2023, which “helps alleviate provider shortages, increases access to mental health services, lowers the cost of care for patients by widening provider networks, and provides timely access to medical care to individuals in rural areas.”
Committee Chair Virginia Foxx (R-NC) elaborated: “Telehealth is a lasting solution to the concerns of accessibility and flexibility, and it’s quickly become apparent that it’s here to stay. The industry has so much room to grow, but only if Congress lets it. The Telehealth Benefit Expansion for Workers Act does just that by allowing employers to offer standalone telehealth coverage.”
ONS Perspective
The U.S. Department of Health and Human Services promotes telehealth as a means to ensure that “the right care is delivered in the right place at the right time. . . . Telehealth and related technologies produce cost-effective, evidence-based improvements in care, including when they are facilitating patients being treated earlier in the course of disease progression, preventing or slowing potentially costly disease or condition progression that would otherwise result in added burdens for patients, caregivers, and family members.”
Ultimately, ONS and the nation’s 110,000 oncology nurses embrace that too, recognizing how technology contributes to progress that solidifies safe and efficient health care. Breaking down barriers for affordable, accessible health care is the goal of health advocacy.