Transitions in Care
For patients and their care teams, transitions are an integral part of the cancer journey. Patients may be moving from inpatient to outpatient care, an acute care setting to a community-based setting, hospital care to nursing home care (https://www.ons.org/cjon/22/6/supplement/transitional-care-methods-and-processes-transitioning-older-adults-cancer), or even active treatment to ongoing survivorship (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8910165/). Care transitions can be times of intense information overload for patients, caregivers, and the healthcare team.
Poor communication and lack of understanding during transition phases can lead to medication errors, adverse events, and hospital readmissions, among other complications. Researchers in one study (https://doi.org/10.37765/ajmc.2021.88622) estimated that 11% of hospital readmissions were preventable with improvements in transitional care planning, among other factors. Within the hospital system, transitions from the intensive care unit to a non–intensive care unit can result in medication errors, with one group reporting (https://psnet.ahrq.gov/issue/evaluation-medication-errors-transition-care-icu-non-icu-location) errors in 46% of cases studied. Improving patient handoffs benefits everyone involved.
Nurse-Led Clinic Clarifies Communication During Transitional Periods
Hospital systems continue to trial a variety of tools and mechanisms to ease care transitions, including implementation of the SBAR (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5123547/) (situation, background, assessment, recommendation form), transitional care models (https://www.jons-online.com/issues/2021/november-2021-vol-12-no-11/4115-bridging-the-gap-achieving-excellence-in-oncology-transitional-care) through nurse navigators, and, in the case of Fox Chase Cancer Center (FCCC) in Philadelphia, PA, the transitional care clinic (TCC). The program is built on the fundamental principle of communication.
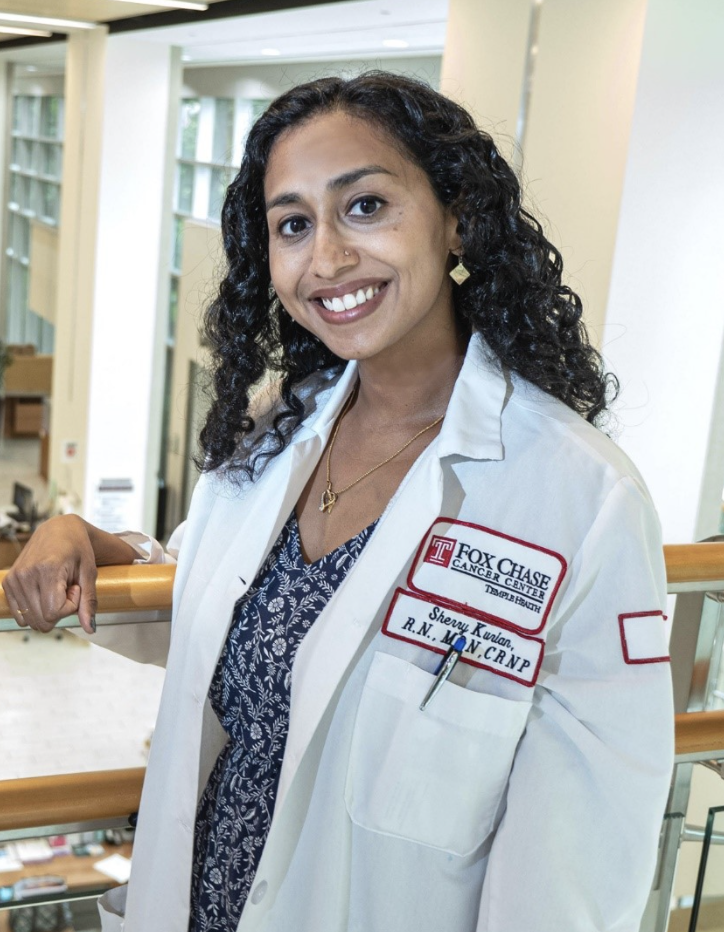
ONS member Sherry Kurian, RN, MSN, CRNP, a nurse practitioner in the hospitalist division of FCCC’s department of medicine, said her institution’s 30-day readmission rates had increased annually for three years, and many patients with ongoing issues well after their hospitalization did not have adequate follow-up care arranged to address these issues. They developed the TCC, a nurse practitioner–driven clinic to bridge the handoff period between the inpatient and community setting for patients with cancer discharged from the hospital.
“After a patient is discharged from the hospital, follow-up with the primary care physician and oncology team varies,” Kurian said. “Changes in medication regimens, treatment plans, management of new drains, and medical devices at the time of discharge can be overwhelming and emotionally exhausting for the patient to manage.” She has encountered many instances where patients and caregivers feel “engulfed with the burden of care” after leaving the hospital.
In addition to supporting patients and caregivers with critical information about their next phase of care, the TCC is also designed to support the care team during transitions, including establishing or re-establishing referrals with community providers and outpatient services.
“The oncology nursing team plays a paramount role in the care transition process for patients with cancer being discharged from the hospital,” Kurian said. Because nurses at the bedside understand the complex needs of the patient, they are able to anticipate and advocate for those needs with receiving providers when patients are transferred to another facility or setting. Nurses working in navigation, case management, and transitional management care also have critical roles during this time.
The nurse practitioner on the TCC care team serves as the patient’s primary point of contact during the care transition to ensure clear and open communication, Kurian said. When transitioning patients to a new provider following discharge, such as an ambulatory or community cancer care team, the TCC forwards the TCC encounter note to the medical oncologist and discharging hospitalist to ensure urgent issues are discussed and resolved with the care team before the actual transfer. Kurian explained that for those urgent conversations, the nurse practitioner will contact providers using the hospital-based secure chat messenger.

Oncology Nurses Are the Linchpin in Transition-of-Care Navigation
ONS member Jackie Miller, MSN, RN, OCN®, director of Oncology Navigation at the Sidney Kimmel Cancer Center (SKCC) at Thomas Jefferson University in Philadelphia, PA, is in the process of implementing a transitional care program at her institution. SKCC is part of an 18-hospital academic health system spanning two states. She explained that the center consists of four advanced cancer care hubs, with a main National Cancer Institute–designated center in Philadelphia. Patients with cancer receive care at multiple locations, often crossing state lines. They may travel some distance to receive care, then obtain follow-up care at a different center.
She said that the program will provide safe handoff and care coordination, address outpatient barriers to care, and educate about next steps and care logistics. By establishing a consistent oncology point of contact, the center can improve team communication, assist with logistics, provide financial advocacy, and help to prevent avoidable hospital readmissions.
At SKCC, the oncology nurse’s responsibilities in the transition of care nurse navigation role are to:
- Participate in oncology unit rounds and team rounds Monday–Friday and in case management discussions for inpatient services.
- Communicate daily with the unit case manager and attending medical oncologist or fellow.
- Collaborate with the ambulatory pharmacist early on to assist in the process of obtaining specialty medications as needed.
- Discuss potential clinical trials with research coordinators.
- Ensure patients are included in the treatment decision-making process.
- Facilitate or support patients and teams in identifying patients’ care goals.
- Facilitate communication between disciplines.
- Reinforce patient education documented in the electronic health record.
- Determine where patients will receive future treatment.
- Collaborate with the outpatient oncology scheduling team to arrange follow-up appointments prior to patient discharge.
- Reinforce the outpatient appointment schedule with patients and caregivers prior to discharge.
- Identify and address barriers to care, prioritizing any barriers for the first outpatient appointment. Refer the patient to support services if appropriate.
Positive Potential for Long-Term Outcomes
Coordinating care among sites and with external providers is complicated, Miller said. As part of the ongoing development and implementation process, the SKCC team is identifying key performance measures to evaluate and share results in the future.
Kurian’s program is also relatively new and awaiting formal evaluation data. However, initial feedback has been positive.
“Although we do not have any numerical data right now, we do see the positive impact of our clinic on an individual level,” Kurian said. “There have been several instances where medical oncologic emergencies were identified early, and early evaluation likely avoided serious complications for the patient. Medication corrections, nutritional support, and referrals to specialists are a few of the common interventions performed at our visits.”
In the future, Kurian said she hopes to collect data that would enable them to compare readmission rates for patients seen in the TCC versus those who missed their appointments, track institutional 30-day readmission rates, and assess improvements in patient satisfaction scores.
Others who have implemented similar programs have had successes. Writing (https://www.jons-online.com/issues/2021/november-2021-vol-12-no-11/4115-bridging-the-gap-achieving-excellence-in-oncology-transitional-care) about a transitional care model implemented at East Carolina University in Greenville, NC, Chelsea Passwater, DNP, RN, AGCNS-BC, OCN®, reported a 9.6% hospital readmission rate after implementing the program, which is lower than the national average of 27% for patients with cancer.
In another study (https://link.springer.com/article/10.1007/s11606-021-07019-6) of a transition clinic implemented in the primary care setting, patients had significantly fewer emergency department visits and hospitalizations within three months of discharge.
Nurses seeking more information on implementing a postdischarge transitional care clinic in their hospitals can start with the Agency for Healthcare Research and Quality (https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/carecoordination/index.html) and Centers for Medicare and Medicaid Services (https://innovation.cms.gov/innovation-models/cctp).
