Oncology APRNs’ Role in Communicating With Older Adults With Cancer
Prepare for the silver tsunami (https://doi.org/10.1158/1055-9965.EPI-16-0133)—experts predict that the number of older adults with cancer, those aged 65 and older, will double by 2035. Oncology APRNs have a pivotal role in their care, understanding patients’ values and preferences to facilitate informed decision-making. But communication can be difficult (https://doi.org/10.1017/S1478951520000218) when patients have comorbid geriatric syndromes (https://ascopubs.org/doi/full/10.1200/EDBK_237641) such as cognitive deficits (https://www.ons.org/pep/cognitive-impairment?display=pepnavigator&sort_by=created&items_per_page=50), delirium (https://voice.ons.org/news-and-views/when-delirium-is-recognized-and-addressed-early-patient-outcomes-improve), and depression (https://www.ons.org/pep/depression?display=pepnavigator&sort_by=created&items_per_page=50).
Effective communication facilitates high-quality conversations, prioritizes patient and caregiver concerns, and helps align their decisions, values, and preferences. Here are three key nursing roles (https://doi.org/10.3390/healthcare11040546) that advanced practice providers can use to support older adults with cancer during the decision-making process.
Geriatric Assessment
Advanced practice RN ( (https://doi.org/10.1200/JOP.2016.017608)APRN)-led geriatric assessments (https://doi.org/10.1200/JOP.2016.017608) (GAs) involve assessing for geriatric syndromes (https://ascopubs.org/doi/full/10.1200/EDBK_237641), identifying patient preferences, and facilitating communication among patients, caregivers, oncologists, and primary care physicians. GAs can help the cancer care team tailor treatment decisions (https://doi.org/10.1188/23.CJON.27-32) according to patients’ preferences and frailty, significantly reduce (https://doi.org/10.1188/23.CJON.27-32) length of hospital stays and postoperative complications, and ultimately improve outcomes (https://doi.org/10.1188/23.CJON.27-32).
In rural settings among patients with low to middle incomes, oncology APRNs have successfully conducted (https://doi.org/10.1200/EDBK_349829) patient self-administered (or caregiver administered) geriatric assessment questionnaires. Several brief geriatric assessment tools (https://doi.org/10.1001/jamaoncol.2020.6736) are available, including the Geriatric-8 (G8) questionnaire (https://www.siog.org/files/public/g8_english_0.pdf) and Vulnerable Elders Survey (VES)-13 (https://www.rand.org/health-care/projects/acove/survey.html).
Providing Information
Oncology APRNs communicate effectively by taking time with the patient and caregiver, exchanging information, and discussing the options for treatment, thereby promoting shared decision-making. However, oncology providers often lack training in older adult–specific communication skills with older adults.
Participation in geriatric oncology cognition and communication skills training programs increases healthcare providers’ communication skills (http://dx.doi.org/10.1016/j.pecinn.2022.100066), knowledge (https://doi.org/10.1016/j.jgo.2023.101484), and self-efficacy perception (https://doi.org/10.1017/S1478951520000218), but incorporating communication, assessment, and decision-making takes practice. See the sidebar for a list and examples of essential communication competencies.
Advocacy
Patients rely on oncology APRNs to fully disclose disease- and treatment-related information that they can use to make decisions. Developing a culture of mutual respect and emotional support is essential to establish that partnership. To advocate for their older adult patients’ wishes when their children are involved in treatment decisions (https://doi.org/10.3390/healthcare11040546), APRNs should focus primarily on the patient, acknowledge all parties’ perspectives, involve the children and the family system, check on understanding, and promote communication between patients and children.
Code status, prognosis, transition to palliative care, and other sensitive topics may lead to difficult conversations, but improved communication can increase patient satisfaction, a metric often used to quantify quality results for reimbursement. In addition to palliative care conversations, effective communication is particularly beneficial (https://doi.org/10.1188/23.CJON.27-32) for advance care planning (ACP) discussions and documentation (https://voice.ons.org/news-and-views/advance-care-planning). ONS’s ACP video (https://www.ons.org/videos/advance-care-planning-video) and worksheet (https://www.ons.org/clinical-practice-resources/advance-care-planning-worksheet) give you additional tools to support your ACP communication for older adults with cancer.
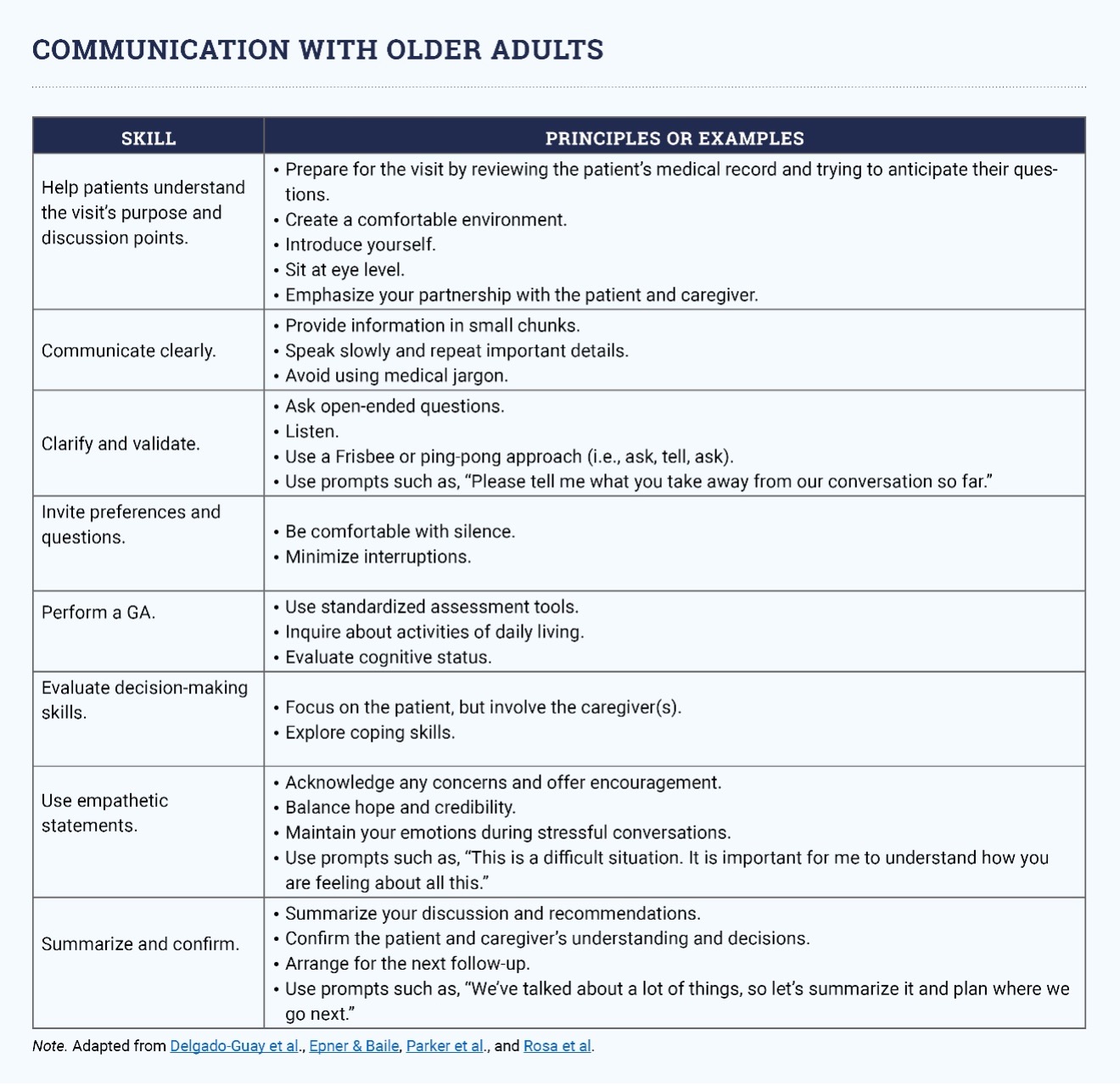
Note. Adapted from Delgado-Guay et al (https://doi.org/10.1093/annonc/mdt263)., Epner & Baile (https://doi.org/10.3109/0142159X.2010.530316), Parker et al (https://doi.org/10.1016/j.jgo.2023.101484)., and Rosa et al (http://dx.doi.org/10.1016/j.pecinn.2022.100066).
