Genetic Disorder Reference Sheet: PTEN Hamartoma Tumor Syndrome
Alterations in the phosphatase and tensin (PTEN) homologue gene result in PTEN hamartoma tumor syndrome (https://doi.org/10.1038/s41431-020-0651-7), which includes Cowden, Bannayan-Riley-Ruvalcaba, and PTEN-related Proteus and Proteus-like syndromes. Pathogenic variants in the PTEN gene are associated with increased risk for developing multiple benign and malignant tumors, some of which may occur in childhood.
Cancer Risks
A person with a pathogenic PTEN variant has an estimated 85%–89% overall risk (https://doi.org/10.1038/s41431-020-0651-7) of developing malignancy and most will have some manifestations by age 20–29 (https://doi.org/10.1111/cge.13875). Pathogenic variants are associated with the following tumor risks (https://www.ncbi.nlm.nih.gov/books/NBK1488/).
|
Tumor Type |
Incidence |
Average Age of Onset |
|
Female breast cancer |
25%–80%, penetrance is 50% by age 50 |
38–50 years |
|
Benign thyroid nodules |
30%–68% |
38 years |
|
Thyroid cancer (usually follicular, occasionally papillary) |
13%–35% |
38 years |
|
Uterine fibroids |
Common |
35–45 years |
|
Endometrial cancer |
20%–30% |
35–45 years |
|
Renal cancer |
15%–35% |
40–49 years |
|
Gastrointestinal polyps, including ganglioneuromas, hamartomas, juvenile, and adenomas |
13%–16% |
30–39 years |
|
Melanoma |
6% |
As young as 5 years |
Testing, Identification, and Early Detection
Prompt identification of people with pathogenic PTEN variants allows providers to implement a complex and aggressive screening and prevention program to decrease their risk for morbidity and mortality. If tumor testing identifies a pathogenic PTEN variant, refer the patient for germline testing. Individuals with a known germline pathogenic PTEN variant in the family should also be referred for counseling and testing.
Clinical presentation of germline PTEN pathogenic variants varies, but guidelines for referral for evaluation (https://nccn.org/) are based on combinations of criteria (https://doi.org/10.3390/cancers11060844).
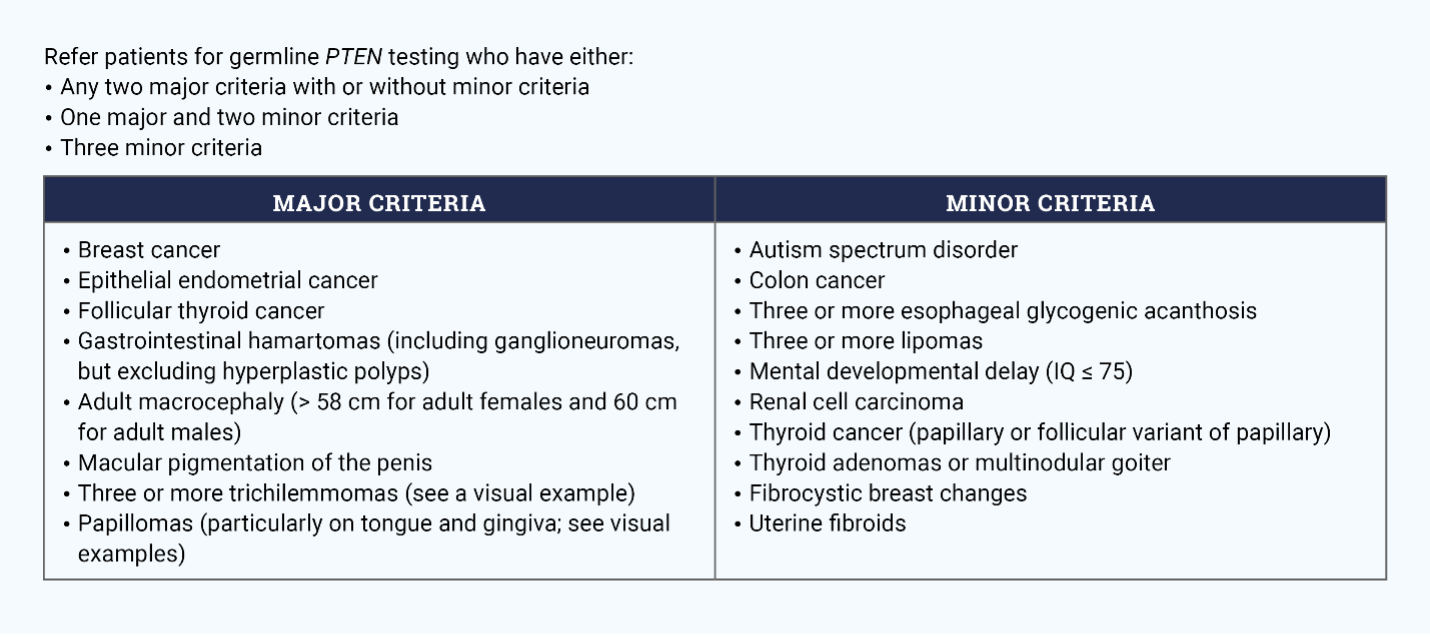
Note: See visual examples of trichilemmomas (https://www.ncbi.nlm.nih.gov/books/NBK1488/figure/phts.F1/) and papillomas (https://www.ncbi.nlm.nih.gov/books/NBK1488/figure/phts.F2/).
The Cleveland Clinic’s PTEN Risk Calculator (https://www.lerner.ccf.org/gmi/ccscore/) is an evidence-based clinical scoring system that providers can use to identify adults for referrals or consideration for research studies. It creates a mathematical model for each patient’s individual factors; those with a threshold probability of 3% or higher should be referred for testing. The tool has a projected sensitivity of 90% for detection of patients with a PTEN pathogenic variant.
Screening and Risk Reduction
People with a pathogenic PTEN variant should follow established management recommendations (https://nccn.org/) that involve rigorous screening (https://www.ncbi.nlm.nih.gov/books/NBK1488/) and consider risk-reducing surgery.
Screening
- Begin annual breast magnetic resonance imaging (MRI) at age 25–29 years; alternate annual mammography and breast MRI every six months at age 30. Conduct a clinical breast exam every 6–12 months starting at age 25. Educate patients on breast self-awareness and prompt evaluation of any change starting age 18.
- Conduct annual transvaginal ultrasound screening of the endometrium and endometrial biopsy starting at age 35. Educate patients to report any unexplained spotting, bleeding, or discharge.
- Obtain annual thyroid examination and thyroid ultrasound starting at age 7 years.
- Begin colonoscopies by age 30 or 10 years prior to the earliest colon cancer diagnosis in the family. Repeat every three to five years or more frequently depending on the polyp burden.
- Consider conducting renal ultrasound every one to two years starting at age 40.
- Conduct annual full body skin examinations starting at age 5.
Surgery
- Surgery reduces the chance of developing breast cancer by at least 95%. Patients and providers may consider bilateral risk-reducing mastectomy with optional breast reconstruction.
- Consider surgery to remove the uterus at age 35–45 years or when childbearing is complete.
Other Prevention Strategies
- Patients should avoid artificial tanning and prevent sunburns by using a broad-spectrum (UVA/UVB) sunscreen of SPF 30 or higher, seeking shade, covering up with clothing (including hats), and wearing UV-blocking sunglasses.
Implications for Nurses
Germline testing and management of individuals with a pathogenic PTEN variant requires ongoing lifetime screening, both of which begin at age 5 (https://www.ncbi.nlm.nih.gov/books/NBK1488/). Families need psychosocial support and a consistent team of providers to implement prevention and detection measures.
