- Advanced Practice Nursing (APRN) (http://dev-voice.ons.org/topic/advanced-practice-nursing-aprn)
- Care Coordination (http://dev-voice.ons.org/topic/care-coordination)
- Patient Support (http://dev-voice.ons.org/topic/patient-support)
- Oncology Nurse Education (http://dev-voice.ons.org/topic/oncology-nurse-education)
New Technology Tools Help Oncology APRNs Improve Patient Outcomes
Clinical decision support systems (CDSSs) are tools (https://doi.org/10.1016/j.soncn.2018.03.007) integrated into electronic health records (EHRs) that include (https://doi.org/10.1038/s41746-020-0221-y) reminders for preventive care, evidence-based clinical practice guidelines, order sets, and alerts for drug prescribing. In health care, artificial intelligence (AI) converts data into knowledge to guide clinical decisions. When combined, the two technologies can guide advanced practice RNs (APRNs) and other providers with predictions and suggestions that go beyond human accuracy and specificity.
Technology Is Better Together
One use for AI-based CDSSs is to predict (https://doi.org/10.1200/JCO2018.78.8687) older adult patients’ risk for falls, sepsis, and chemotherapy toxicity. APRNs and other providers may also use them to connect patients with clinical trials based on their molecular profiles. When used in oncology, CDSSs can lead to increased (https://doi.org/10.1016/j.soncn.2018.03.007) quality and satisfaction with care, improved health outcomes, and reduced cost of care. Engaging patients while using AI and CDSSs may also promote (https://cancer.jmir.org/2021/4/e31616) better communication, shared discussions, and informed treatment decisions.
AI and CDSSs in Advanced Practice
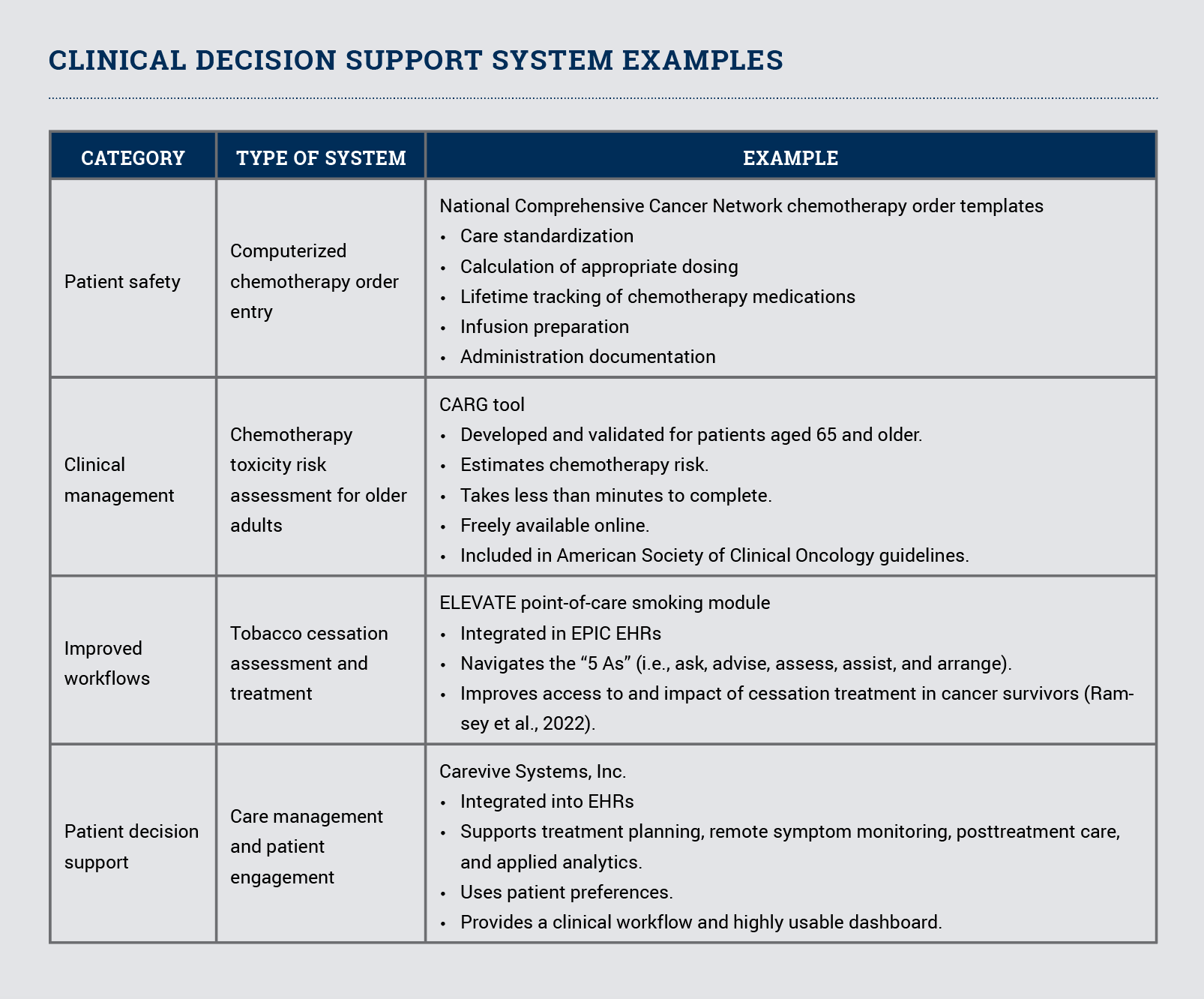
Oncology APRNs can use CDSSs and AI in all phases of practice: defining clinical problems, training, implementation, and evaluating impact. Integrating CDSSs into a practice (https://doi.org/10.1177/0825859718810723) setting starts with interprofessional collaboration among stakeholders to determine feasibility, function, advantages, barriers, and priorities. Many of those tools are already incorporated into EHRs or easily added; see the sidebar for examples of various systems. Cost is often the primary barrier, but oncology APRNs and implementation teams can support adoption with strategic planning and emphasizing how CDSSs improve patient outcomes.
APRNs Are Leading the Way
The integration of the Cancer and Aging Research Group (CARG) tool into practice is an example of how oncology APRN are leading this effort. When our practice participated (https://doi.org/10.1016/j.jgo.2019.05.005) in the Oncology Care Model and City of Hope’s R25 geriatric oncology nursing education program, we realized the value of embedding the tool in our EHR to improve care for older adults receiving chemotherapy.
We identified stakeholders from nursing, information systems, oncology practice, and the medical oncology fellowship program and developed a six-week process from inception to completion. Now we use the CARG tool in clinical practice to assess chemotherapy toxicity risk in older adults and built the findings into tumor board presentations and discussions. There was no cost to integrate the tool, and it’s led to quality improvement and better care for older adults with cancer receiving chemotherapy.
Shared Decision-Making Tools Facilitate Patient-Centered Care
Patient decision support tools, such as Carevive and ONS On-Call (http://ons.org/licensing-opportunities/on-call)TM, are readily available, and many integrate with patients’ personal health records (PHRs). PHRs involve a two-way relationship whereby providers transmit information to patients and patients can enter information for their providers.
Many PHRs used for symptom tracking and can assist providers in symptom triage and management. Disparities such as computer or broadband access and digital literacy may be barriers for patients and providers, but as use of telehealth and teleoncology explodes, so does the opportunity to routinely implement AI, CDSSs, and PHRs in practice.