Launched in 2016 as a pilot program from the Centers for Medicare and Medicaid Services (CMS) Innovation Center to develop new payment and delivery system models, the Oncology Care Model (OCM) had a lofty goal: drive improvements in providing high-quality and cost-effective care.
The program concluded in June 2022, and its outcomes created both success stories and opportunities for healthcare providers and practices. Although the OCM promoted value-based care, after making all the performance-based payments, Medicare showed a net loss. Now oncology practices are awaiting the next model with the hope that CMS will continue to incentivize and reward patient-centered, affordable care.
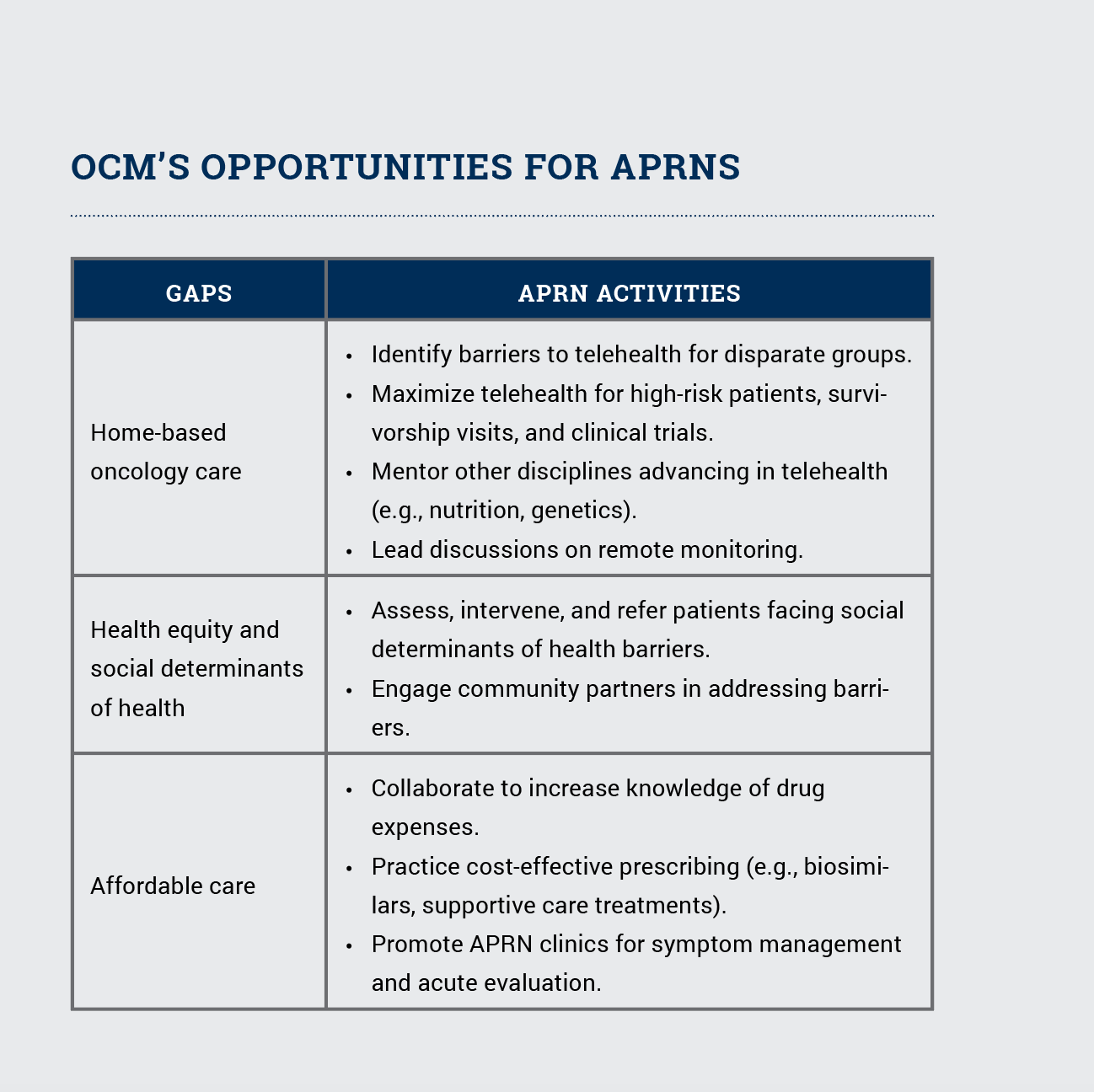
As we reflect on the OCM’s achievements and acknowledge where it fell short, advanced practice RNs (APRNs) have opportunities to build on successes and spearhead improvements.
APRNs’ Role in OCM’s Success
Areas where APRNs helped to influence positive practice transformation included care delivery, symptom management, patient-centered care, and end-of-life care. They transformed how cancer care is delivered by improving triage and creating acute care clinics. They taught patients to call first instead of going to the emergency department and offered same-day clinics to manage acute symptoms.
APRNs have also helped organizations overcome the challenges of standardizing the use of evidence-based guidelines and balancing effectiveness. They improved organized and patient-centered care with navigation and documenting care plan components. APRNs have also led discussions with patients for shared decision-making, advanced care planning, palliative and hospice care, and referrals for supportive care.
How APRNs Can Improve Today’s Cancer Care
APRNs are key providers who can revolutionize telehealth and teleoncology care through remote monitoring, survivorship visits, clinical trials, and mentoring other interprofessional team members (e.g., nutrition, genetics). APRNs can also lead the promotion of health equity and attention to the social determinants of health that affect oncology care. Social and economic disparities have become more apparent under the OCM, and improvements in assessment and intervention will help overcome barriers to care, including clinical trials and telehealth.
Among their communities, APRNs can reduce barriers to care, help patients navigate the healthcare system, and improve outcomes. Working on those factors now may achieve long-term benefits if future models incentivize community engagement to address social care issues. The OCM also gives APRNs new opportunities to learn about the costs of care, implement care pathways, and consider biosimilars for precision medicine.
APRNs have been at the forefront of patient-centered care and can further advance their role through lessons learned with the OCM. See the sidebar for specific strategies APRNs are using to close the gaps and continually improve cancer care.
Future Applications
In addition to the OCM’s impact on medical oncology, CMS will implement the Radiation Oncology Model (ROM) in January 2023, now creating opportunities for radiation oncology providers to show value and quality of care.
Like with the OCM, patient experience is an important quality measure in the ROM. A difference, however, is that the ROM is mandatory whereas OCM was voluntary, and the program is case based versus bundled for payment.
To meet the ROM, practices must submit biannual clinical data for five tumor types: bone, brain, breast, lung, and prostate cancer. The model also assesses four quality measures:
- Radiation and medical oncology plan of care for pain
- Radiation oncology treatment summary communication
- Assessment, treatment, and follow-up for depression
- Advance care plans
Medical oncology APRNs who have experience with the OCM have another opportunity to guide radiation oncology staff and APRNs as they begin the ROM.






