Oncology Nurses Have a Role in Genomics Throughout the Cancer Care Continuum
By Kathleen A. Calzone, PhD, RN, AGN-BC, FAAN
Cancer genomics influences all oncology nursing roles. Walking through the cancer care continuum shows (https://pubmed.ncbi.nlm.nih.gov/23368676/) how genomics—and oncology nursing—are involved at every level.
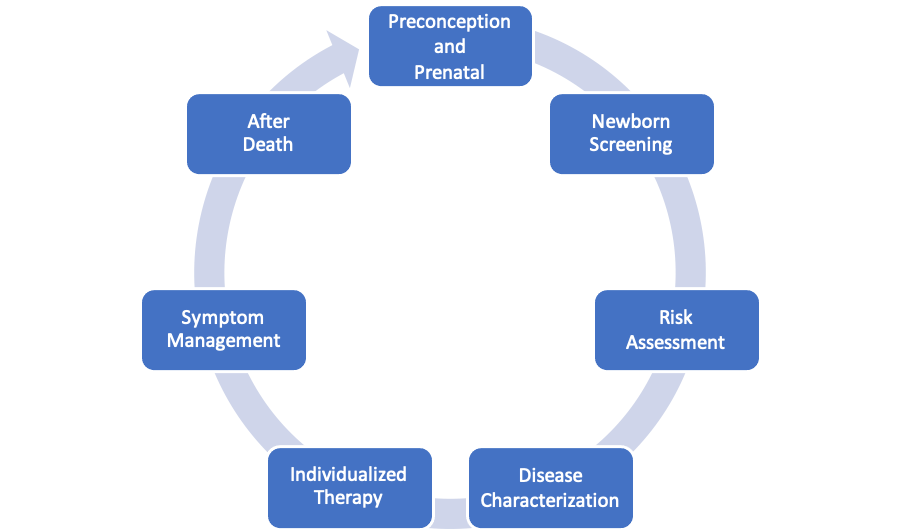
Preconception and Prenatal
Patients harboring germline pathogenic variants in cancer susceptibility genes may inquire (https://doi.org/10.1007/s10689-013-9685-0) about preimplantation genetic testing during preconception to prevent transmitting the pathogenic variant to their children. After conception, the introduction of noninvasive prenatal screening using cell-free fetal DNA decreased the requirement for chorionic villus sampling or amniocentesis, which are risky. Although rare, cell-free fetal DNA testing has identified (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5823781/) evidence of malignancy in the mother.
Newborn Screening
Tests using dried blood spots from a newborn heal prick look for evidence that further genetic evaluation is required. Researchers are exploring (https://doi.org/10.1016/j.ajhg.2018.11.016) the accuracy, feasibility, and ethics of DNA sequencing as part of newborn screening. How does this affect oncology nursing? Identifying a germline pathogenic variant in a cancer predisposition gene results in lifelong implications for the newborn, but adult family members will also now require education and counseling about testing for that specific variant.
Risk Assessment
Genomics has expanded beyond standard genetic variants that confer risks for breast and colon cancers. Cancers thought to be primarily environmental in nature, such as mesothelioma, are now associated with a wide range of germline pathogenic variants in tumor suppressor genes. Discoveries (https://doi.org/10.1097/JTO.0000000000000130) such as these have therapeutic implications (https://doi.org/10.1073/pnas.1821510116) that affect all oncology nurses.
Screening
Take colonoscopy as an example. Despite its high sensitivity and specificity for preventing or finding colorectal cancer early, adherence rates are often low because patients are reluctant to undergo the test preparation. A less-invasive stool DNA testing, which received U.S. Food and Drug Administration approval (https://www.accessdata.fda.gov/cdrh_docs/pdf13/P130017b.pdf) in 2014, is an alternative screening test (https://link.springer.com/article/10.1007/s10620-014-3451-5) that may overcome that patient barrier. Oncology nurses can help educate patients about their screening options.
Disease Characterization
Genetic analyses can identify tumor characteristics that may influence therapeutic decisions or germline testing recommendations, such as in microsatellite instability (MSI). Done at the at the time of pathology review, testing enables clinicians to look for evidence of DNA repeats indicative of MSI. When coupled with immunohistochemistry to assess protein loss, testing can help identify (https://doi.org/10.1158/0008-5472.CAN-16-1637) whether MSI is from a germline variant (which would indicate patients should follow up with germline testing) or epigenetic DNA methylation.
Individualized Therapy
Tumor genomics such as MSI or somatic sequencing are used (https://doi.org/10.1186/s13046-019-1094-2) to identify patients who are candidates for targeted therapy based on driver genetic variants. This area of cancer genomics continues to evolve (https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-017-1290-9) as we learn more about things such as tumor genetic heterogeneity (single tumors with different genetic changes throughout the tumor) and disease progression (tumors can be resequenced at the time of progression to identify additional genomic changes that could be used as new therapeutic targets).
Symptom Management
Throughout it all, oncology nurses have vital roles in education, support, care delivery, and symptom management. Additionally, nurse scientists are elucidating (https://doi.org/10.1016/j.critrevonc.2017.11.012) the genomics of symptoms, which may one day help us identify patients at risk for certain symptoms and improve management.
After Death
The progress we’ve seen from applying genomics throughout the cancer care continuum is the result of biospecimen research. Given DNA stability (the Neanderthal was sequenced) and easy storage, biorepositories are fundamental to research. With consent, genomic analyses can occur at any time, including after death. Some analyses may identify germline findings with clinical implications for biologic family members. Patient would need to sign a release (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4617203/) to permit the posthumous testing and to specify who would receive the information. Both the prospective release as well as coordinating family notification involve the oncology nurse.
From administration to navigation, care delivery, counseling, education, research regulation, informatics, and scientific investigation, genomics intersects with all oncology nursing roles, and the practice implications span the entire cancer care continuum.
