What Happens During a Genetics Counseling Session?
When referring patients for genetics counseling (http://aboutgeneticcounselors.com/) and possible testing for hereditary risk, oncology nurses can help relieve their trepidation and anxiety by explaining what to expect during the visit. See the sidebar for key indications for referral.
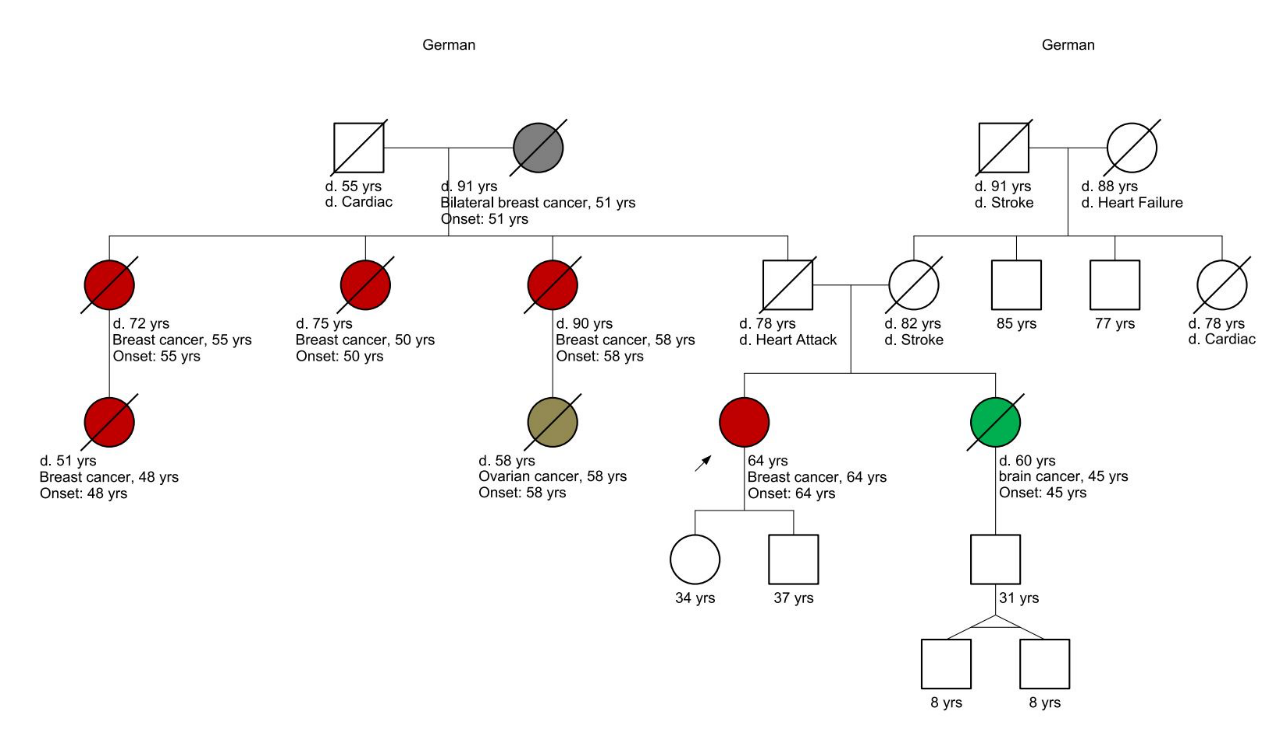
Building a Pedigree
Prior to the visit, a genetics professional (https://www.genome.gov/FAQ/Genetic-Counseling) will ask the patient to gather their maternal and paternal family history, including information about the ages or age at death and health (including age and site of cancer diagnosis) of children, siblings, parents, grandparents, aunts, uncles, cousins, and nieces or nephews. Patients should also collect any prior genetic testing results from any of those family members. This information is critical to the evaluation.
The genetics counselor will also ask questions about their ancestry, because some ethnic groups are at higher risk (https://www2.tri-kobe.org/nccn/guideline/gynecological/english/genetic_familial.pdf) for hereditary cancers. The genetics professional will draw all of the collected information into a pedigree (https://www.genome.gov/genetics-glossary/Pedigree) (see sidebar). The accuracy of the pedigree determines the accuracy (https://doi.org/10.1188/16.ONF.655-660) of the risk calculations and recommended genetics tests and gene panels.
Counseling Patients
Once the pedigree is complete, the genetics professional will evaluate it and meet with the patient to discuss how it affects their cancer risk. Most initial visits will last 60–90 minutes.
Often testing is recommended, but not always; when not recommended, patients might require more vigilant screening. If a family mutation has not yet been identified, the genetics professional will try to identify the best family member in whom to initiate testing. Ideally, a family member who has been diagnosed with cancer—whether in active treatment or cured of the disease—has the highest likelihood for a positive result. Once a family mutation is identified, other family members can usually have testing only for the specifically identified mutation. However, every family is different, and the genetics professional will help each family select the best test (https://doi.org/10.6004/jnccn.2019.7343) based on both sides of their family history.
If genetic testing is an option, the genetics professional will discuss the benefits, risks, and limitations and give patients and family members the opportunity to ask questions and discuss concerns. This discussion is very important to ensure the patient and family have enough information to make an informed decision and are prepared for any consequences. They have many considerations to weigh, including the possible outcomes and what it might mean for other family members. Individuals must decide whether testing is best for them or if they would be better off not knowing if there is a mutation.