Telehealth Visits During COVID-19
With the Centers for Disease Control and Prevention’s recommendations for practicing social distancing (https://www.cdc.gov/coronavirus/2019-ncov/about/prevention.html) to slow the national risk of transmission of COVID-19 novel coronavirus, oncology nurses must take increased precautions with patients with cancer who are at increased risk (https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications.html) for contracting or experiencing poorer outcomes from COVID-19. Patients require communication and education in these uncertain times.
Using Telehealth to Maintain Care
Clinicians should consider implementing novel practice changes to protect patients while still providing excellent care. Telemedicine is being increasingly used when evaluating and treating patients for COVID-19, and similar strategies can be used in cancer practices for routine symptom management and other non-urgent follow-up or survivorship visits. Using telehealth or other alternative remote communication options may reduce the volume of patients coming to the office in an overburdened system as well as limit possible COVID-19 exposure for high-risk patients. Patients can preemptively be screened for respiratory illness and referred to the appropriate provider if indicated before coming to appointments.
Commercial programs are available, or practices can develop their own programs. Offices should encourage use of electronic patient portals for nonmedical questions and telephone triage calls to evaluate symptoms.
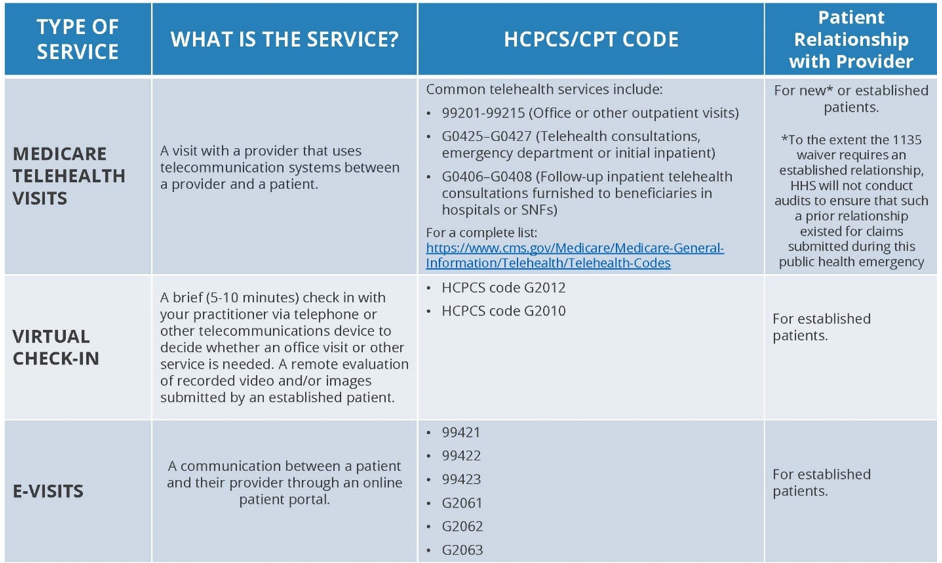
Billing Telehealth Visits
On March 6, 2020, Congress passed the Coronavirus Preparedness and Response Supplemental Appropriations Act (https://www.congress.gov/bill/116th-congress/house-bill/6074/text), part of which temporarily waives Medicare requirements for telehealth visits (https://www.cms.gov/newsroom/press-releases/covid-19-response-news-alert-cms-issues-frequently-asked-questions-assist-medicare-providers) during the current public health emergency, which historically had several restrictions. On March 17, 2020, the Centers for Medicare and Medicaid Services (https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet) (CMS) released a telehealth expansion that allows providers to bill for virtual visits that use both audio and video components in patient homes for any demographic region. CMS also allows payments for virtual check-ins or e-visits, which encourage use of telephone encounters and patient portal communication (see chart).
Commercial payors are increasingly supportive of telehealth, encouraging synchronous virtual care using live videoconferencing and other options as a valuable and often preferred option, and prior restrictions are being reduced. If necessary, patients can be provided with other alternative scheduling approaches such as postponing appointments for long-term, lower-risk follow-up visits or grouping and separating appointment times for the highest-risk patient groups. Make sure patients understand the strategies and precautions that are being taken to protect them.
By providing increased communication and education using traditional and alternative or remote appointment options like telehealth, clinicians will be able to help ease anxiety, provide effective assessment and management of patients, and reduce COVID-19 exposures to patients and staff.