Central line-associated bloodstream infections (CLABSIs) can cause serious harm or even death to patients and significantly increase healthcare costs. Nurses are critical contributors to infection prevention in any healthcare setting, particularly for oncology’s often-immunocompromised patient population, ONS member MiKaela Olsen, DNP, APRN-CNS, AOCNS®, FAAN, clinical program director for oncology at the Johns Hopkins Hospital and Johns Hopkins Health System in Baltimore, MD, said.

Factors Related to Central Line Infections
Olsen explained that CLABSIs are related to two time points: insertion and maintenance. Insertion-related CLABSIs are laboratory-confirmed bloodstream infections not associated with an infection at another site that develop within 48 hours of central line placement. However, most infections are classified as maintenance-related because they occur after time. When Olsen’s team evaluated maintenance-related infections among Johns Hopkins’ patient population, it found that they often correlated with frequent and difficult dressing changes.
“Dressing longevity affects the rate of infection,” Olsen said. “The more frequently that you need to remove and reapply the dressing, the more you are exposing the insertion site and threatening skin integrity. Our goal is to maintain a transparent dressing that is clean, dry, and intact with no blood for seven days.”
Johns Hopkins’ procedure involves applying a hemostatic agent during every central line insertion to avoid additional dressing changes. For maintenance, nurses are trained to look for bleeding with each dressing change and daily during assessments. They also use a hemostatic agent to stop any bleeding and prevent infection. If bleeding is not present, they use a chlorhexidine-impregnated dressing to prevent infection.
“CLABSI prevention should include daily rounds by nursing leaders, infection control, or other designated staff to assess dressing integrity and ensure they are clean and dry,” Olsen said. “Abnormal findings should be communicated immediately to frontline staff so they can make timely corrections.”
Although the nurses have extensive competency and skills validation, Olsen said, if the central line is inserted in a less-than-ideal location (e.g., excessive skin folds, hair growth), preventing infection can be a losing battle. Those who insert the lines are taught how to choose the best insertion site, avoid areas near other tubes and drains, and properly secure the line.
“The decisions made during insertion might not cause an immediate infection but can affect maintenance of the line the entire time it is in,” Olsen said. “For example, when a line is placed in the jugular vein and extends up the neck near the ear, by the hairline or beard, and we can't keep a dressing on or secure it properly, then we’re going to have a constant struggle maintaining the dressing,” she said.
Difficult Dressings May Require Special Tools and Tactics
That’s when it’s time to bring in what Olsen calls the “SWAT” team. Each site at Johns Hopkins has a full-time, at-the-ready team of experts who are specially trained in vascular access and exclusively manage all aspects of central line insertion and maintenance, including difficult dressings. Nurses call them at the first sign of a problem so they can bring their knowledge, skills, and tools to address it.
Her team also developed a difficult-dressing guide that includes tips to handle common scenarios, such as sweating and bleeding. The goal is to empower direct care nurses. “But, if they’re having trouble, they can escalate it and we send somebody in,” Olsen said.
Dressings are not the only factor which contributes to CLABSI, but they are an example of a situation that is always escalated if the site cannot be kept clean, dry, and intact, Olsen said.
Set Up a System to Stop Infections
Olsen co-chairs Johns Hopkins’ Vascular Access Device and Central Line–Associated Blood Stream Infection Reduction committees, which work collaboratively with representatives from six hospitals in the system. Because they work at different sites, nurses communicate through a secure chat in the electronic health record and include a picture of the challenging dressing; at some sites, a nurse rounds on all central lines daily to make sure proper measures are in place to prevent infection.
Establishing a process to encourage escalation of concerns, provide bedside support, and promote a culture of safety could allow Johns Hopkins’ method to work in any system, Olsen said. As the nursing profession faces limited nursing resources and high turnover, having a dedicated team can help ensure quality.
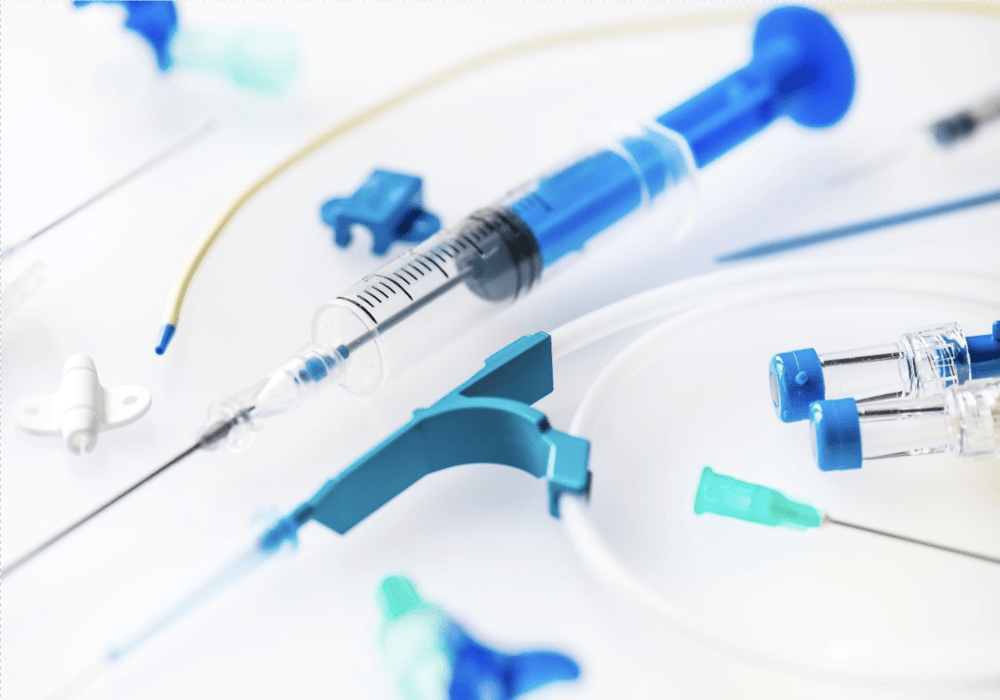
If an institution doesn’t already use one, Olsen encouraged building a central line dressing change kit that contains all of the tools to perform one correctly. Olsen’s institution worked with a vendor to provide a kit for sterile dressing changes from start to finish, including a small sterile drape, sterile gloves, two masks, chlorhexidine, skin barrier solution, alcohol pads, and central line dressing. Individual items are unpackaged but remain sterile, saving valuable nursing time.
Finally, Olsen reminded nurses that patients and caregivers are important members of the infection prevention team, especially when they are changing their own dressings. Patients are encouraged to call the telephone triage nurses if they are having trouble with dressing longevity and provided with answers to frequently asked questions, including:
- What a CLABSI is and how it is treated
- What healthcare providers do to prevent CLABSIs
- Tips to prevent infections, such as telling providers immediately if the bandage becomes wet or dirty or the area becomes sore
- Advice for family and friends about proper handwashing practices and avoiding touching catheters or tubing