A well-known and well-liked patient on the oncology unit, Ms. M, had been responding well to a treatment regimen for metastatic cancer but had a rare side effect from one of the chemotherapy drugs: progressive and paralyzing extremity weakness. The condition was nonreversible and painful, and no treatment could slow its progression.
The Ethical Dilemma
Ms. M told her nurse that she did not want to be placed on a ventilator if it became necessary, but she wanted to be kept comfortable. However, her family was upset with the healthcare team because they thought her cancer was going away and the treatment caused this life-threatening condition. The physicians spoke to the family about potential options such as a ventilator and resuscitation but did not talk to Ms. M regarding her wishes, even though she was of sound mind. The family asked that she be intubated but kept on the patient care unit and not transferred to the intensive care unit. The patient did not want this and for ethical, legal, and safety reasons, this request could not be honored. The family refused to make a do-not-resuscitate order (DNR), despite her wishes and declining status. Her family held onto the faith that a cure was available to reverse her condition. Because the physicians did not want to take away hope, they were reluctant to order a DNR. The nurses were distressed about the lack of a DNR, and the physicians were distressed that the therapy caused her condition and were unwilling to let go.
The Nurse’s Role in Overcoming Medical Futility
Rubin defined medical futility as treatment that does not achieve a patient’s goals. The impression of medical futility arises when the involved parties’ values do not match. Nurses bring their own morals, beliefs, and past experiences when caring for patients, and families may not have the same values as the healthcare team or even the patient. Medical and moral debates are made from all parties’ perspectives.
Research has shown that futile care is a continual source of stress in nursing. Nurses report that some of the highest-identified hindrances to good end-of-life care include disagreement about the path of dying patients’ care, prolongation of suffering, and physicians’ reluctance to address the reality of the situation with families. They also identify family factors such as lack of understanding of patients’ conditions and what can or cannot be done, not accepting a poor prognosis for their loved ones, and overriding patients’ wishes, including advance directives.
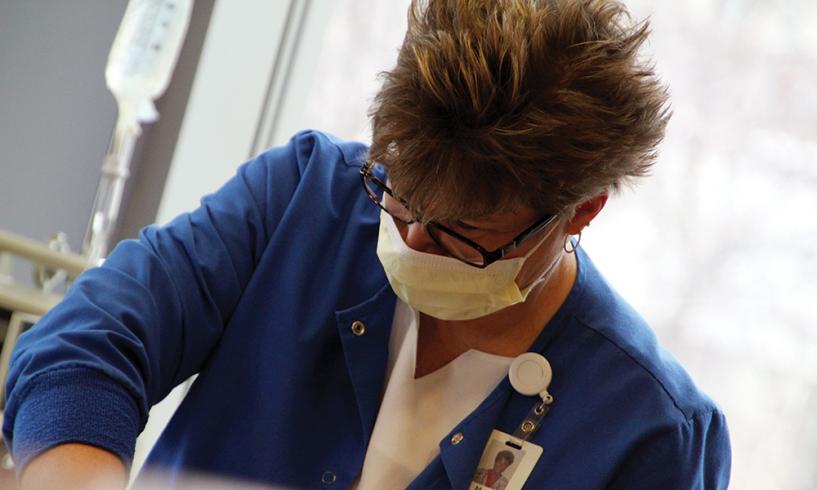
When conflicts arise, ethics committees, interdisciplinary team communication, collaborative practice, and institutional policies can help guide decisions. Oncology nurses act as liaisons between patients, families, and providers, and the nurse’s role is to provide comfort care, advocate, and clarify information.
In Ms. M’s situation, the healthcare team and family eventually came to an agreement and honored her wishes. She died comfortably several days later with her family at the bedside.