Spiritual care is an essential component of cancer care. Representing an individual’s “sense of peace, purpose, and connection to others and beliefs about the meaning of life, spirituality is not synonymous with religion, which is “a set of beliefs and practices that center on questions about the meaning of life and may involve the worship of a supreme being.” Several healthcare organizations such as the National Comprehensive Cancer Network, American Society of Clinical Oncology, Multinational Association of Supportive Care in Cancer, and the Joint Commission recommend including spiritual care in cancer care guidelines.
Benefits and Barriers to Spiritual Care
Many patients with cancer place a personal significance on their spiritual and religious views and want to talk about it. Benefits of spiritual care include improved quality of life, satisfaction with care, and patient-provider relationships. However, when their spiritual needs are not addressed, patients experience more distress, anxiety, and feelings of hopelessness.
Because of barriers such as lack of training and confidence, lack of time, and social, religious, or cultural differences between patients and healthcare staff, oncology advanced practice providers (APPs) may not routinely provide spiritual care. Student training programs and oncology competency programs for practicing nurses and clinicians should consider using online and blended learning approaches to incorporate spiritual care.
Challenges in Decision-Making
Spiritual or religious beliefs have a direct effect on patients’ decision-making for treatment and supportive care and may lead to raise ethical, legal, and medical challenges for oncology providers. For example, patients who are Jehovah’s Witnesses may not accept blood products, and other religions may have beliefs that affect decision-making about pregnancy, complementary and alternative medicine, clinical trials, reconstructive surgery, and end-of-life considerations. Oncology APPs need to consider how religion and spirituality may affect treatment and supportive care for all of their patients.
Spiritual Care Assessments
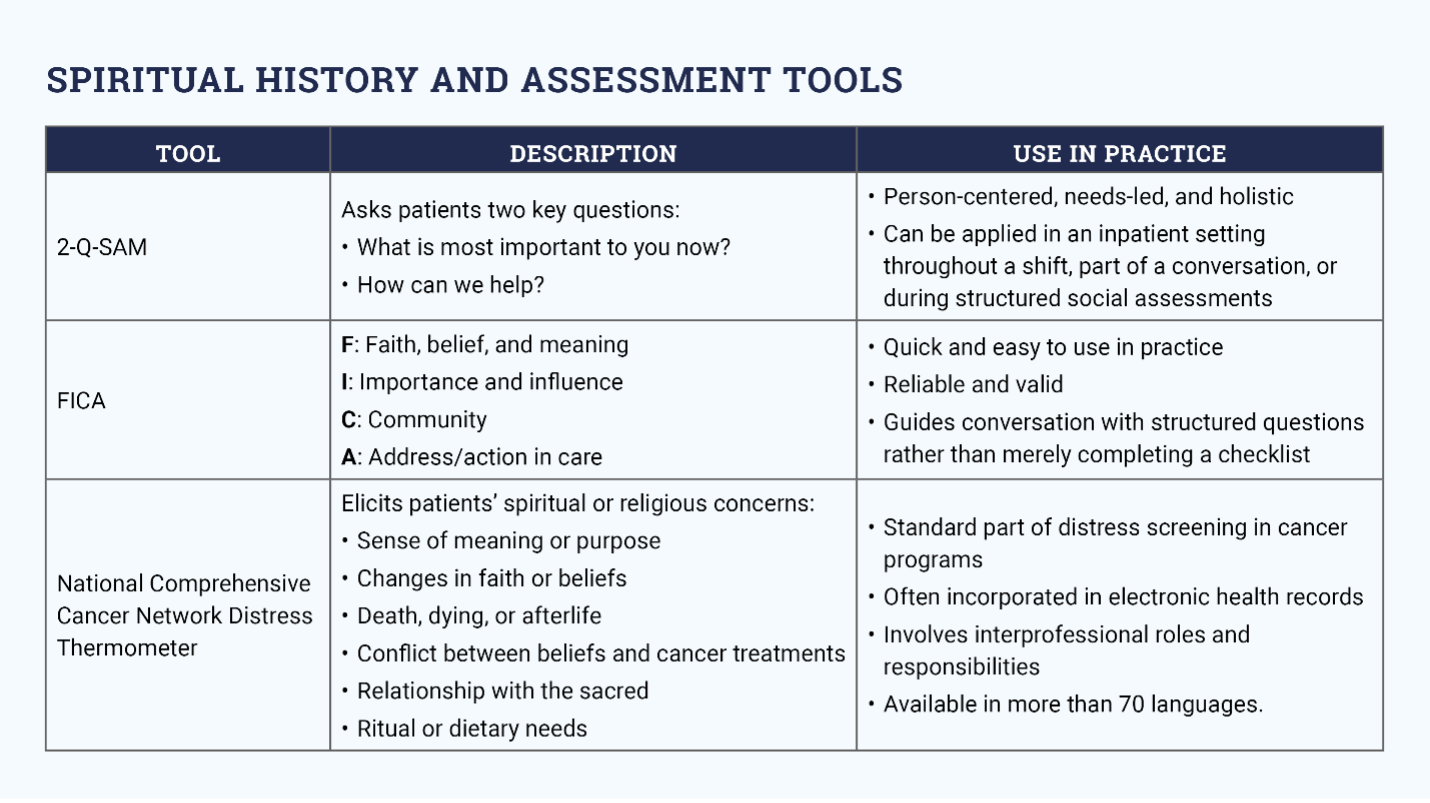
Oncology APPs can identify a patient’s religion and spirituality through spiritual care assessment tools (see sidebar) at various points throughout patient encounters, such as while taking their social or personal history or when reviewing distress screening tools. Assessing spiritual and religious needs is important on initial as well as follow-up visits, particularly if patients are experiencing distress because of clinical status changes, pain, or other changes from previous visits.
Interventions
Allowing patients to share their story or life review is an evidence-based way to promote spiritual well-being. Oncology APPs can facilitate aspects of life reviews even during brief encounters by engaging therapeutic communication techniques, including compassionate presence in a quiet space, reflective listening, and open-ended questions to guide conversation.
Clinicians should work in close partnership with trained spiritual professionals (e.g., chaplains, pastoral care advocates) and make prompt referrals. Oncology APPs can also recommend that patients use self-care practices to explore and express their spirituality, such as meditation, support groups, and spiritual readings. Additional nursing resources for spiritual care are listed in the sidebar.