The CHEK2 (checkpoint kinase 2) tumor suppressor gene provides cells with instructions for making a protein known as CHK2, which becomes active when the cell’s DNA is damaged or strands of it break. CHEK2 halts cell division and enables either cell repair or destruction. Without a properly functioning CHEK2 gene, cells lose a key restraint on their growth which may lead to uncontrolled cells and possibly malignancy. CHEK2*1100delC is the most common pathogenic variant and most prevalent in European populations.
Cancer Risks
Germline CHEK2 pathogenic variants are associated with an increased risk for developing a variety of cancers, including female and male breast, colon, prostate, gastric, pancreatic, kidney, and thyroid cancers and, less commonly, brain tumors and sarcomas.
The CHEK2 gene is considered a moderate risk penetrance gene, meaning that a person who carries a pathogenic variant has a two- to threefold increased risk of developing a malignancy than someone without it. Genetic counseling for those individuals is challenging because their risk is elevated, but the exact extent varies depending on the pathogenic variant and family history. A detailed family medical history is essential to identify potential risks and guide screening recommendations.
For example, a woman with a pathogenic CHEK2 variant has an estimated 17%–40% overall risk of developing breast cancer, compared to 12% in the general population. Women with a breast cancer diagnosis or a strong family history of breast cancer may consider risk-reducing mastectomy. No consensus guidelines are available, and shared decision making is important.
The specific pathogenic variant may also influence risk. The I157T pathogenic variant, another common CHEK2 variant, is associated with a higher risk for developing colon cancer.
Nursing Implications
Individuals with a pathogenic CHEK2 variant require ongoing screening. Knowledge about how pathogenic CHEK2 variants affect prognosis is emerging. CHEK2*1100delC carriers tend to develop ER-positive tumors, have a worse overall survival, and are at higher risk for contralateral breast cancer, which might affect surgical decision-making. Because the exact risks are not fully understood, screening recommendations involve family medical history. Regular consultation with a genetics professional enables carriers to stay updated on current recommendations.
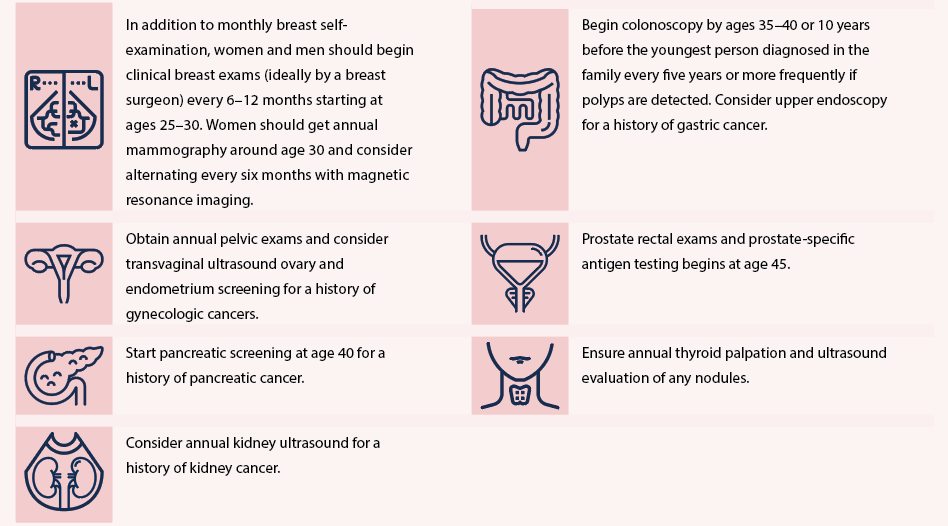
Note. Based on information from National Comprehensive Cancer Network and Tung et al.