Although the burden of a cancer diagnosis is a profound experience for patients, healthcare systems often fail to address patients’ and families’ psychosocial, information, and care coordination needs. Patient navigation programs, specifically those provided by oncology nurse navigators, have been introduced to help address these care gaps. In their article in the February 2013 issue of the Clinical Journal of Oncology Nursing, Horner et al. describe the oncology nurse navigator (ONN) program at their institution. They address the specific roles of nurse navigators, required training, resources involved, and lessons learned.
Developing a Nurse Navigator Program
Horner et al.’s (2013) program was developed as part of a National Cancer Institute-funded study comparing the use of ONNs to enhanced usual care. Initially, the researchers planned to include three oncology nurses on the ONN team; however, the final team consisted of nurses from medical oncology, general surgery, and breast cancer screening. Horner et al. found that the diversity of background ended up being a strength of the program, because the nurses could share medical expertise and process knowledge across departments.
The nurses maintained their work in their departments and served as ONNs for about eight hours per week. Each nurse could manage a maximum of eight navigation patients at any one time. Before meeting with patients, the nurses received training that reinforced their current skills and reviewed psychosocial skills, including
- Empathic and motivational enhancement communication strategies
- Depression assessment
- Behavioral activation
- Problem-solving strategies for distress.
Day-to-Day Work
ONNs strived to meet each of their patients in person and attend one or more of their medical appointments with them. They felt this allowed them to develop a more trusting medical relationship with the patients. After the initial meetings, nurse-initiated phone calls were made weekly to assess patients’ status and needs. Patients were also given the number for the ONN’s dedicated cell phone to call or leave a message at any time.
An ONN who was also a clinic nurse said that the key difference between the two roles was that ONNs provided proactive care by asking patients about their concerns and problems at regularly scheduled encounters, whereas clinic nurses responded reactively to incoming queries from patients for immediate triage or problem solving.
The ONNs used the National Comprehensive Cancer Network’s distress thermometer to assess patient problems. For each area of distress, ONNs identified the perceived source and developed an action plan to address it. Action plans often included multidisciplinary interaction, such as scheduling an appointment with a patient’s primary care provider to discuss antidepressants or referring patients to genetic counseling.
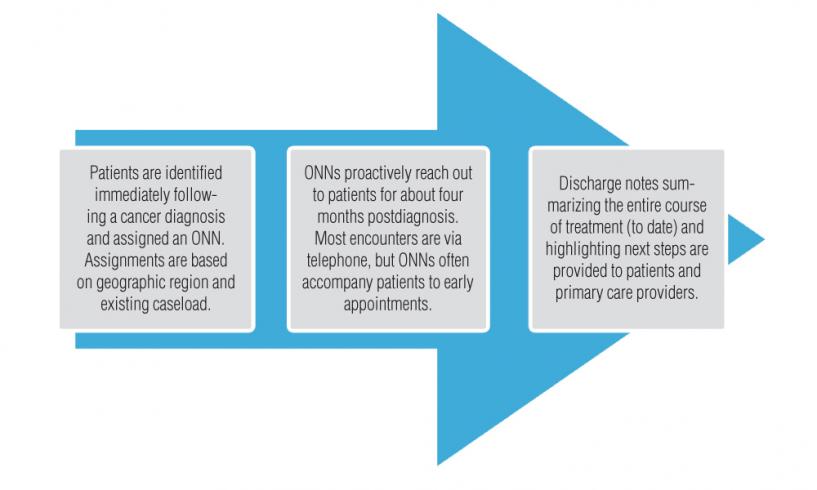
For a flowchart of the ONN’s work with each patient, see Figure 1. A complete list of the ONNs’ roles and responsibilities is in Table 1.
Lessons Learned
After the ONNs had been in the role for two years, Horner et al. saw that several key themes emerged as lessons learned from the program.
- The severity of patients’ illness does not necessarily indicate the intensity of their distress. Personality, family support, financial situation, employment, and previous healthcare experiences all contribute to how patients handle their cancer.
- Healthcare providers should listen more and talk less. Listening carefully from the start allows patients to fully explain what their needs are.
- Weekly calls with patients gave ONNs the opportunity to reinforce treatment accomplishments and offer clinical and psychosocial support for patients when they feel stressed or stuck by a particular problem.
- The intimacy of the relationship allows for more comprehensive patient understanding than is seen in usual care, allowing them to make more informed decisions about care.
In addition to lessons learned about patient interaction and care, the ONNs also found some surprising revelations about themselves and their personal nursing practice.
- “The program helped me to mature as a nurse,” one navigator said, “to discuss the whole patient, not just the disease.”
- Another described her key takeaway as learning how to teach patients to problem solve, providing the appropriate resources for assistance.
- “The first step to being a good nurse is to listen with compassion and empathy to really hear what the patient is saying,” the third navigator summarized.
For more information on the navigator program, including two case studies demonstrating the ONN role and outcomes, refer to the full article by Horner et al. Five-Minute In-Service is a monthly feature that offers readers a concise recap of full-length articles published in the Clinical Journal of Oncology Nursing (CJON) or Oncology Nursing Forum. This edition summarizes “An Oncology Nurse Navigator Program Designed to Eliminate Gaps in Early Cancer Care,” by Kathryn Horner, MS, Evette J. Ludman, PhD, Ruth McCorkle, PhD, RN, FAAN, Ellen Canfield, BSN, RN, Lynn Flaherty, RN, BSN, ONC, Jennifer Min, RN, BSN, Janice Miyoshi, BS, Beth Lapham, BA, Erin J. Aiello Bowles, MPH, and Edward H. Wagner, MD, MPH, which was featured in the February 2013 issue of CJON. Questions regarding the information presented in this Five-Minute In-Service should be directed to the CJON editor at CJONEditor@ons.org. Photocopying of this article for educational purposes and group discussion is permitted.